Chronic Pain
Living with chronic pain affects everything your mood, sleep, mobility, and daily comfort. At Solis Medical Clinic, we take the time to understand your story and what you’re going through. With compassionate care and evidence-based treatments, we help you manage your pain, regain confidence, and get back to the life you want. Your path to feeling better starts here.

Understanding Chronic Pain
Chronic is pain that lasts or comes and goes (recurs) for more than three months. Pain is usually a symptom, so your medical doctor needs to determine what’s causing your pain, if possible.
The World Health Organization (WHO) in its 11th revision of the International Classification of Diseases (ICD-11) includes chronic pain as a diagnosis in its own right, further categorizing chronic primary pain and chronic secondary pain. Chronic primary pain refers to pain that exists despite complete tissue healing, or pain that has no identifiable cause. Chronic secondary pain occurs in association with underlying diseases (e.g., rheumatoid arthritis).
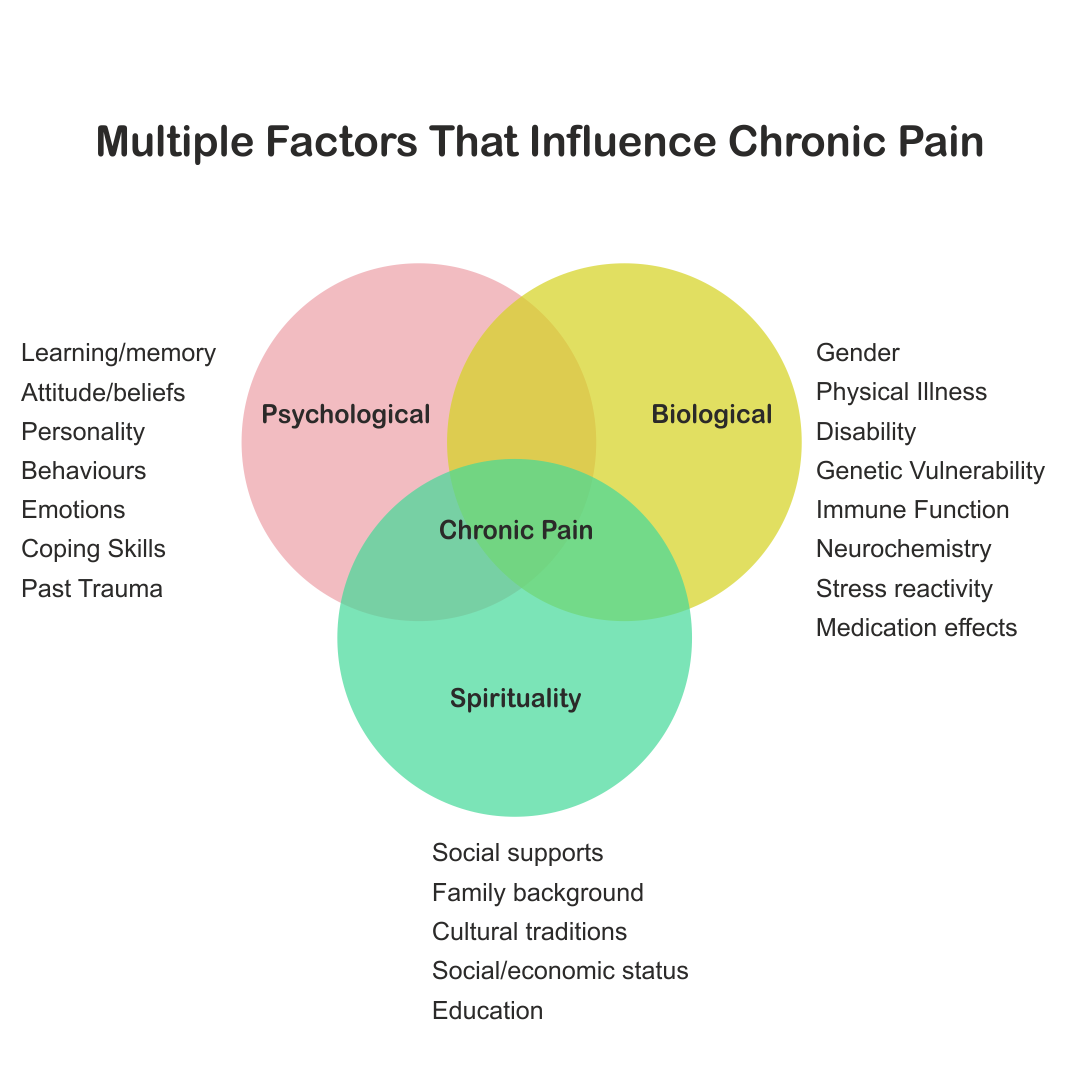
Factors That Influences Chronic Pain
Biological, psychological, spiritual, environmental, and social factors influence our experience of pain. Chronic pain, like other chronic diseases, is best understood within a biopsychosocial framework, and its treatment should integrate pharmacological, physical, psychological, spiritual, self-management, and other approaches, as appropriate.
Chronic Pain Assesment
A chronic pain assessment involves a comprehensive evaluation that includes a patient’s pain history, its impact on daily life, and a physical examination. This evaluation can take an hour or more. Key components are a thorough medical history detailing pain characteristics (onset, quality, location, severity), an assessment of how pain affects daily functions and emotional well-being, and a physical exam to validate the history.
What We Ask During Your Consultation:
At Solis, we will be asking you about your past medical history that includes your mental health history and previous emotional trauma. We ask about current medications and over the counter supplements. We will also inquire about your response to previous medications and any other interventions.
You are asked to come in 15-20 minutes early to fill out forms that include some pain assessment tools.
You will first meet our nurse then the pain specialist.
A pain assessment, like all medical evaluations, serves two main purposes
-
 To understand the nature of the pain problem and its confounding factors.
To understand the nature of the pain problem and its confounding factors.
-
 To provide a baseline against which the effect of treatments can be measured. This second aspect is often more difficult than for many medical problems where outcomes are often simpler to recognise.
To provide a baseline against which the effect of treatments can be measured. This second aspect is often more difficult than for many medical problems where outcomes are often simpler to recognise.
For pain problems, improvement in ‘pain’ may, paradoxically, not be the main endpoint, but improving how the pain is understood and managed may be the essential outcomes. This means, we try to help you function better despite having chronic pain.
At Solis, we strive to provide patient education, understanding and expectations about chronic pain.
At Solis, we use the 6 pillars of chronic pain management to help guide treatment. These pillars include medication, lifestyle changes, psychological intervention, physical therapy, injectable interventions, and spirituality.

Injectable Options
Please always eat a light meal and hydrate well before any injection therapy. For your safety, we do not do injections if you have an active infection. We encourage you to make your follow up appointment before you leave the clinic.

Trigger point injections
A trigger point injection can help soothe myofascial pain, especially in your jaw, neck, shoulder, arms, legs and lower back.
Trigger points are painful “knots” in your muscles that can be very sensitive to touch/pressure. They may form after acute trauma or by repetitive micro-trauma, leading to stress on muscle fibers. It causes the muscle fibers to be stuck in a contracted state. Sometimes you can feel these knots when you rub your muscle.
Trigger point injections commonly involve injections of a dilute solution of local anesthetic mixed with magnesium, B12 and sometimes dextrose or ketorolac.
What are trigger point injections used for?
Trigger point injections are a common and generally safe way to treat myofascial pain caused by trigger points. Although the procedure can be temporarily painful, the injection can provide pain relief for a few days to a month if not longer.
The pain and tenderness in myofascial pain are typically due to one or more trigger points. To the touch, trigger points feel like small bumps, nodules or knots in your muscle.
Trigger points can develop in any muscle, but the most common muscle groups that are treated with trigger point injections include: Masseter, Temporalis, Trapezius, Rhomboids, Sternocleidomastoid, Levator Scapulae, Gluteal Medius, Thoracic and lumbar paraspinals.
Trigger points can cause certain types of pain or issues. For example, trigger points affecting your trapezius muscle may cause tension headaches. A trigger point affecting your piriformis muscle (a muscle in your buttocks) can cause piriformis syndrome — when the piriformis muscle presses on your sciatic nerve. It causes pain or numbness in your buttock and down the back of your leg.
Who needs to have a trigger point injection?
A trigger point injection may be right for you if your trigger point pain has not improved with other treatments, including over-the-counter pain medication, heat therapy, massage therapy, myofascial release and physical therapy.
Trigger point injections are more successful when used alongside with physical therapy and stretching exercises to alleviate the pain.
This strategy can be particularly beneficial when a trigger point injection is initially used to reduce pain in people who are unable to do physical therapy or stretching due to intense pain. The trigger point injection can allow physical therapy to be more effective.
Treatment Details
What do I need to do to prepare for a trigger injection?
There’s nothing you need to do to prepare for a trigger point injection. However, as with any type of treatment, it’s important to discuss your current medications, symptoms and overall health with your provider before getting the procedure.
What happens during a trigger point injection procedure?
You can expect the following during a trigger point injection procedure:
- Depending on the trigger point location, you may be sitting or lying down on an exam table.
- Your healthcare provider will cleanse your skin on the affected area with an alcohol pad.
- Your provider may mark the trigger point. They may use an ultrasound machine to help locate the muscle.
- Once your provider has identified the trigger point by feeling it, they’ll pinch the point between their fingers and stabilize the tissue. This may feel uncomfortable.
- They’ll insert a thin needle attached to a syringe to inject into the trigger point.
- You’ll likely feel your muscle spasm or twitch.
- The procedure will be over, and you’ll be able to go home.
How painful is a trigger point injection?
Trigger points are typically painful to the touch, so you’ll likely experience some pain when your healthcare provider is manually locating the trigger point before the injection.
You may feel a stinging and burning sensation when your provider inserts the needle and medication. When the tip of the needle touches the trigger point, you may feel a brief increase in your pain. Although this may be uncomfortable, this pain is a good sign that the needle is in the correct spot.
What should I expect after a trigger point injection?
After a trigger point injection, you can go home and can actively use the affected muscle. However, you should avoid strenuous activity for the first few days.
What are the benefits of trigger point injections?
Trigger point injections are generally safe and can provide pain relief to people who have been experiencing pain associated with trigger points and have not found relief using more conservative treatments, like over-the-counter pain medication or physical therapy.
Trigger point injections can also provide significant improvement in range of motion and overall muscle functionality, depending on which muscle is affected.
What are the risks and side effects of trigger point injections?
Trigger point injections are generally safe and carry a low risk of complications. The most common side effect is temporary discomfort or numbness around the injection site. You can also apply ice packs or heat to injection sites to reduce the risk of bruising. There is a 1:500,000 risk of pneumothorax if the needle penetrates to deeply into the lung. This is a rare occurrence.
Other complications of trigger point injections, which are rare, can include the following:
Bleeding, Infection, Bruising, Allergic reaction to the anesthetic agent, and Vascular (vein) injury.
How long do trigger point injections last?
Most people experience pain relief starting between 24 and 72 hours after the trigger point injection procedure. Pain relief typically lasts for about a few days to month. Most people need a series of trigger point injections every 2-3 weeks that gradually get spaced out further and further until you no longer require
Complications
If you’ve received a trigger point injection and are experiencing signs of infection, such as a fever, redness, swelling, warmth at the site of the injection, contact us right away or call your family physician. Always make sure to have a follow up appointment.

Prolotherapy
Prolotherapy (proliferation therapy) is a regenerative injection treatment using irritants like dextrose to stimulate the body’s natural healing, encouraging new collagen growth to strengthen weakened tendons, ligaments, and joints, thereby reducing chronic pain from musculoskeletal issues like joint instability or tendinopathy. It works by triggering mild inflammation to kickstart tissue repair, often requiring multiple sessions for gradual strengthening and improved function.
How it works
A solution, usually dextrose (a sugar) mixed with a local anesthetic like lidocaine, is injected into painful, weakened connective tissues (ligaments, tendons).
The solution acts as a mild irritant, causing localized, controlled inflammation, unlike cortisone which suppresses it.
This inflammation signals the body to send repair cells, promoting the production of new collagen and strengthening the tissues, which stabilizes the joint and reduces pain.
What it treats
- Chronic joint and ligament pain
- Tendon strains and sprains
- Joint instability
Chronic arthritis
advantages of prolotherapy
- Pain reduction: Some people who’ve used prolotherapy report a noticeable reduction in their pain after their injections.
- Very few side effects: Prolotherapy is a relatively low-risk treatment that usually doesn’t have any serious side effects.
- Can be used with other treatments: You should also be able to use prolotherapy in addition to other treatments and techniques to manage your pain, but make sure to talk to your provider before starting it.
risks or complications of prolotherapy
- Fortunately, prolotherapy has no serious side effects. You might experience some pain at your injection site, and bruising is rare. There’s a very low risk the injections damage nerves, joints or other tissue near the injection site, but prolotherapy isn’t riskier than any other injection. Make sure you receive prolotherapy from a certified healthcare provider to minimize your chances of complications.
- If you’ve received a prolotherapy injection and are experiencing signs of infection, such as a fever, redness, swelling, warmth at the site of the injection, contact us right away or call your family physician.
Prolotherapy Treatments occur at intervals usually every 4-6 weeks.
Before the Appointment
Avoid anti-inflammatory medication for two days prior and 5 days after your injection. (Anti-inflammatory medications include Advil or Ibuprofen, full strength Aspirin (325 mg), Aleve or Naproxen, Prednisone, steroids, other NSAIDS such as Celebrex or Arthritis .
During the Appointment
The doctor may administer a single injection or a series of injections depending on the region of the body. Sometimes ultrasound guidance is used to locate the area to be injected.
After the Appointment
Depending on the area treated and the number of injections, most patients can return to usual activities during the next day to 2 days. Approved medications or acetaminophen (Tylenol) may be taken for discomfort following injections. Most people can drive after the procedure but occasionally some people are very prone to faintness so if you are, please arrange for someone to drive you home after the treatment. Watch for signs of infection, including increasing pain, redness and swelling that lasts more than 48 hours. Don’t use a bathtub or hot tub for two days, however you may shower. You may experience some bruising on the site.

Botox
Botox is used therapeutically to relieve chronic pain from migraines. Patients who respond well to off-label Botox treatment. Often have:
Frontal headaches
involving the forehead and brow muscles
Temporal headaches
from clenching or overuse of the temporalis muscle (often TMJ-related)
• Occipital or cervicogenic headaches
starting in the neck or suboccipital region
TMJ symptoms
such as jaw tension, bruxism (teeth grinding), ear pressure, or facial tightness
Headaches from Whiplash injuries (after a MVA)
such as jaw tension, bruxism (teeth grinding), ear pressure, or facial tightness
Myofascial pain in shoulders and back.
such as jaw tension, bruxism (teeth grinding), ear pressure, or facial tightness
What to Expect
- Onset: Botox takes 2 weeks to work and usually lasts 3 months
- Procedure: The procedure takes less than 15 minutes. you can return to normal activities, work and most activities immediately after treatment. To reduce redness, swelling or bruising:
- Don’t rub or put pressure on the treatment area for 12 hours.
- Don’t rub or put pressure on the treatment area for 12 hours.
- Avoid physical exertion for 24 hours.
Possible Botox Side Effects
Side effects are rare but include:
- Flu-like symptoms.
- Headache.
- Neck Pain
- Upset stomach (indigestion).
- Temporary droping eyelids (ptosis)..
- Eye irritation or redness.
Botox Treatment is given at 3 months interval

Cortisone (Steroid) injections
Cortisone shots (steroid injections) deliver a dose of medication directly to a problem spot in your body. The cortisone calms your immune system’s response in that location. This reduces pain and inflammation. They can help you manage symptoms or conditions that make it hard to participate in all of your day-to-day activities. By reducing the pain, the hope is to get you back moving and exercising.
Cortisone injections are used in the following conditions. At Solis, we have ultrasound to help guide injections.
Arthritis, Tendinitis, Tendinopathy, Bursitis, Carpal tunnel syndrome, Tennis elbow & Trigger finger and trigger thumb
The most common side effects of cortisone (steroid) shots include:
- Pain at the injection site.
- A temporary increase in swelling.
- Bruising.
- Temporarily increased blood sugar levels. People with diabetes should check their blood sugar level more often for about five days after a cortisone shot.
- Discoloration or redness on your skin at the injection site.
- Skin lightening or looking paler near the injection site.
It’s rare for steroid injections to cause severe side effects, but it’s possible to experience:
- Infections at the injection site.
- High blood pressure (hypertension).
- Fluid retention and increased swelling.
People who receive many rounds of steroid injections may have an increased osteoporosis risk.
Patients with bleeding disorders or on anti coagulants (blood thinners) have increased risk of bleeding.
When should you not get a steroid shot?
- You shouldn’t receive steroid injections if you have an infection. Corticosteroids have a short-term immunosuppressant effect and can make it harder for your body to fight an infection and heal itself.
It takes 10-14 days to see the full benefit of a cortisone injection. Cortisone injections should last three months or more.
Always follow up with your doctor after the injection. Call right away if you are experiencing any signs of worsening pain for infection.

Viscosupplementation
Viscosupplementation is a procedure where a fluid called hyaluronic acid is injected into a joint. Hyaluronic acid lubricates the joints. Pain relief can occur as early as 2 weeks after the injection. Viscosupplementation helps retore joint movement and strength.
It can offer up to 6 months of relief by supplementing the body’s natural joint fluid. The stabilized HA formulation that lasts longer in the joint than natural HA, potentially delaying surgery and improving mobility, and is suitable for those not getting relief from oral meds or physical therapy.
Viscosupplementation can be used in people with mild to moderate osteoarthritis. It has also been uses in severe OA when patient is awaiting joint replacement. It can also be used to treat tendon issues.
Most people don’t have any problems from viscosupplementation.
These injections are done under ultrasound guidance in our Clinic.
The most common problem you might have is a flare-up of your arthritis just after your injection. This might cause more pain and swelling in the short-term.
Less common risks include:
Bleeding
Allergic reaction.
Pain at the injection site.
Infection (delay your injection if you have any active infection to help prevent this).
There is also a chance that the treatment will not help your symptoms. Talk with your provider about all your concerns. Your own risks may vary according to your health conditions and where and how often you get injections.
You should be able to go home shortly after your procedure. Ask your health care provider if it’s OK for you to drive. For the next 48 hours, don’t stand for long periods. Don’t do lots of walking, jogging, or lifting heavy weights.
Some people have slight pain, warmth, and swelling right after their procedure. These symptoms often don’t last long. Using an ice pack may help. Tell your provider right away if these symptoms don’t go away soon. Also tell them if you have severe warmth, redness, pain, or fever.
Don’t expect the injection to ease your symptoms right away. It may take a few weeks to notice a difference. Symptom relief may last for a few months.
If this treatment doesn’t ease your symptoms, you may be able to repeat the injection or series of injections in 6 months or so. But the procedure doesn’t help everyone. If it doesn’t work for you, talk with your specialist.

Other Injectable Options
At Solis, we partner closely with our radiology colleagues to get other interventional treatments you may need such as facet injections, epidural injections, RFA. There are some procedures that are better done under fluoroscopy than ultrasound.